Inflammation and pain following cataract surgery are not only uncomfortable for patients but also inhibitory to proper visual recovery. Fortunately, recent advances in cataract surgery have reduced safety concerns and improved outcomes for patients. Along with these improvements in surgical techniques, a range of medications designed to prevent and treat inflammation following surgery are being developed. An education module from Healio – Opthalmology identified the importance of continuing education for cataract specialists to remain knowledgeable of the most effective options available for treating patients.
Inflammation and pain following cataract surgery are not only uncomfortable for patients but also inhibitory to proper visual recovery. Fortunately, recent advances in cataract surgery have reduced safety concerns and improved outcomes for patients. Along with these improvements in surgical techniques, a range of medications designed to prevent and treat inflammation following surgery are being developed. An education module from Healio – Opthalmology identified the importance of continuing education for cataract specialists to remain knowledgeable of the most effective options available for treating patients.
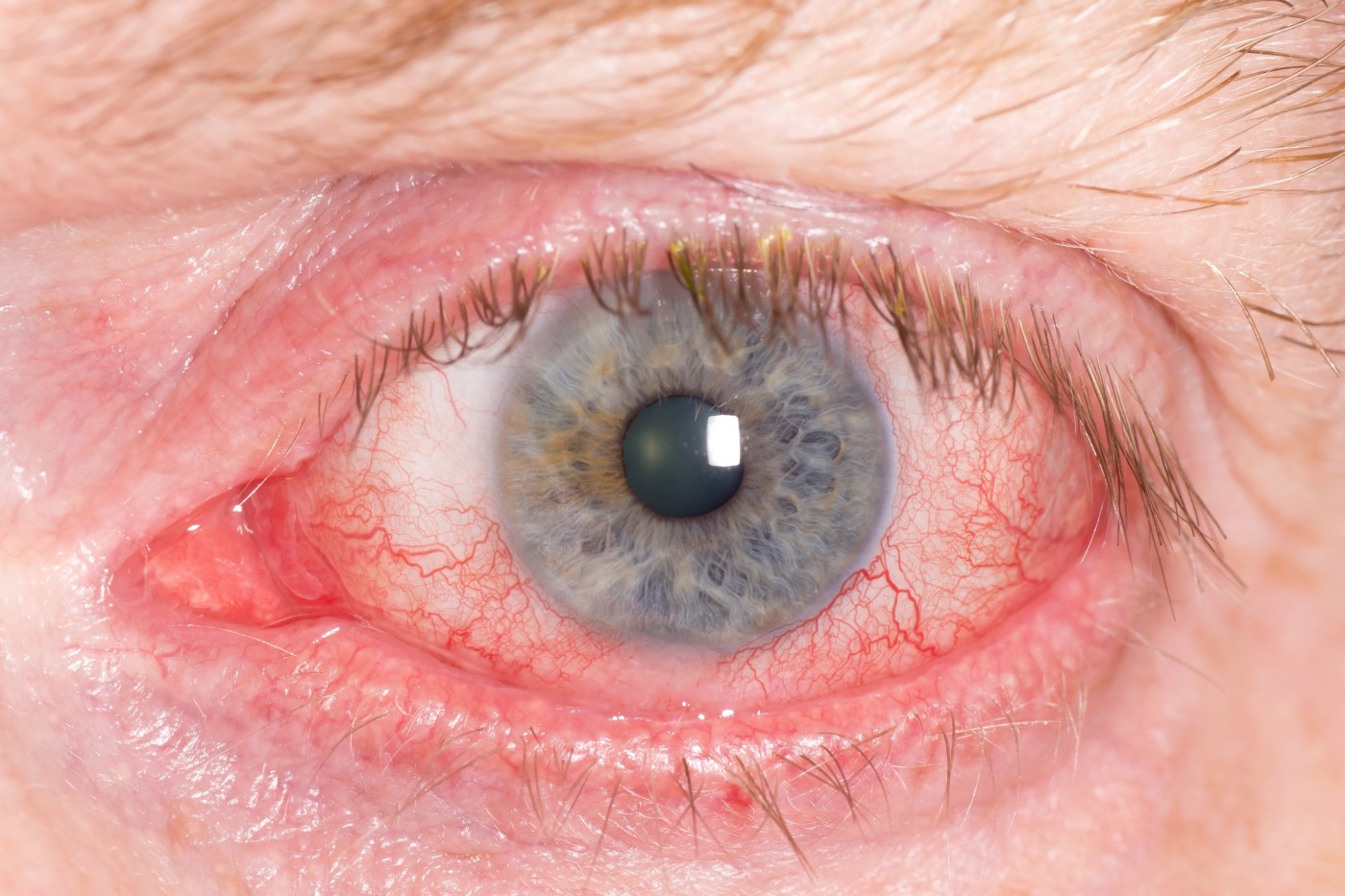
“Patients expect their cataract surgery to go well and recovery to be uncomplicated and pain-free,” stated William B. Trattler, MD, in the article “Postcataract Surgery Inflammation and Pain: Prevention and Treatment.” Unfortunately, these expectations are not always met, and patients may experience complications as a result of inflammation following cataract surgery.
At times the cause is a direct result of the surgical procedure. An 80-year-old man who had cataract surgery returned to the eye doctor with persistent fluid buildup in the cornea (known as a corneal edema). His doctor suspected a nuclear chip, or a fragment of the lens left behind from surgery, and detected the chip using a slit lamp exam. The chip was readily removed after a follow-up surgery.
Corneal edema can signify other complications of cataract surgery. A particularly difficult case involved an 85-year-old man who had reduced vision three weeks after surgery. He showed signs of corneal edema and was instructed to follow a medication regimen to clear up the inflammation but likely did not comply with treatment, delaying his recovery.
Other cases are not as predictable. One 76-year-old woman who underwent implantation of a monofocal intraocular lens following removal of her natural lens came back to the clinic with less than optimal vision, achieving a maximum acuity of 20/30 with corrective lenses. During an examination of her eye, her doctor found cystoid macular edema, or fluid buildup in the macula. This was surprising, as the patient had surgery no more than two weeks earlier, and cystoid macular edema usually develops at least four to six weeks post-operation.
All of these complications were treated with a common medication: nonsteroidal anti-inflammatory drugs (NSAIDs). “The benefits of prophylactic NSAID treatment for cataract surgery patients have been established, while regimens continue to vary,” stated Dr. Trattler. ” Management plans include a range of possible preoperative treatment durations, use on the day of surgery, and duration of postoperative treatment.” Clinical trials are also underway to investigate the use of topical steroids for treating inflammation and pain caused by cataract surgery. Results of previous trials have identified a reduction in intraoperative and postoperative discomfort for patients using NSAIDs when undergoing cataract surgery.